I want to apologize for leaving on a cliffhanger for the past few months! My health has stabilized enough that I am able to hold a part time job. I am now the school nurse at Kitty Bungalow Charm School for Wayward Cats. Learning a new job has been a challenge, and I focused most of my mental and physical stamina learning these past few months. So thank you for being patient with me!
By February of 2015 I was still not tolerating solid food, I had lost 10 lbs, and I was taking Reglan, Phenergan, and Zofran around the clock to control my nausea. My pain had significantly improved since surgery, but I had debilitating nausea and vomiting daily. I would feel full after eating very little, and sometimes hours later I would vomit what despite the nausea medication. I also required frequent hospitalization for intractable nausea and vomiting. During this time I also experienced what I believe was a chemical pregnancy, which is a very early miscarriage when the embryo is lost shortly after implantation. I missed a period, and a home pregnancy test was positive. However a week later a blood test was negative for pregnancy. My gastroenterologist agreed that my Gastroparesis required the care of a motility specialist.


The motility specialist wanted to confirm that Gastroparesis was the true root of my nausea and vomiting, and ordered a SmartPill Motility Test. The SmartPill test has a similar sensitivity to the Gastric Emptying Scan that is the gold standard for diagnosing Gastroparesis, but it doesn’t require sitting in the hospital for 4 hours waiting on the scan and it also measures motility through the entire GI tract. I had a Gastric Emptying Scan in 2008 that diagnosed Gastroparesis. The SmartPill is an electronic capsule that is taken orally after ingesting a standardized meal. It tracks pH, transit time, and temperature through the GI tract and transmits the information by low-wave radio frequency to a data recorder worn by the patient for up to 5 days. The SmartPill test confirmed delayed gastric emptying or Gastroparesis. It also demonstrated that the pill was abnormally re-fluxing between my intestine and stomach.
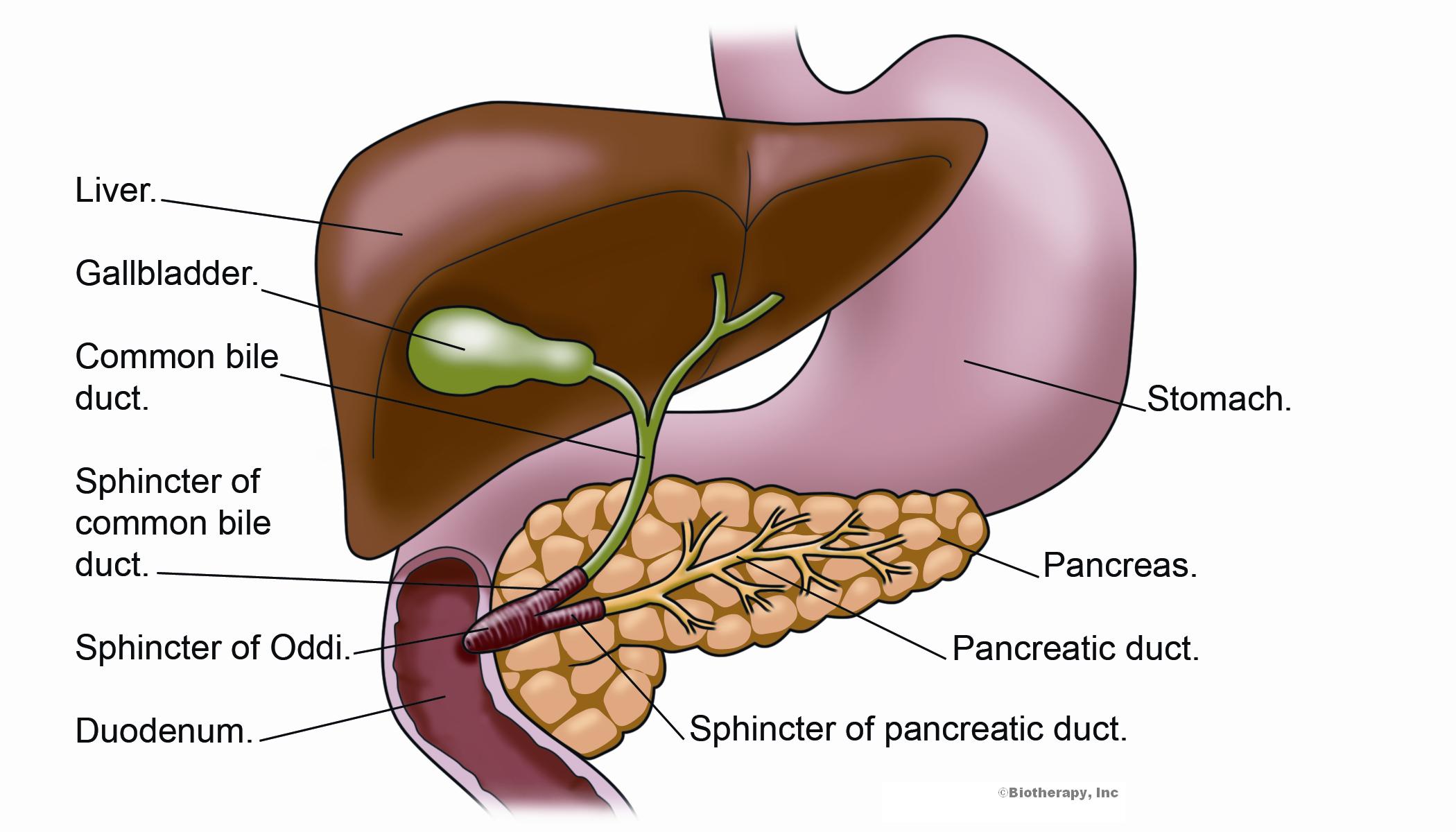
My motility specialist recommended I try a Botox injection into the pyloric sphincter, the muscle that controls the transit of food from the stomach to the small intestine. Botox is a toxin formed by a bacteria knows as Clostridium botulinum, that causes paralysis of muscles; This toxin is the same kind of Botox used in cosmetic procedures to reduce the appearance of wrinkles. It is theorized that injecting the toxin and paralyzing the pylorus would allow food to move more easily from the stomach to the small intestine thus easing the symptoms of Gastroparesis. However, in large randomized controlled trials of Idiopathic Gastroparesis, this treatment was not better than a placebo. However I still felt it was worth a try, but my doctor told me to set realistic expectations. Soon after the procedure I ended up hospitalized again with intractable nausea and vomiting, suggesting the procedure failed to work.
In May of 2015 I watched as my medical class graduated and moved on to residency. I felt left behind, and it was hard to accept that my life wasn’t following the same timeline as those around me. I had one thing that kept me going; I was pregnant again! During my pregnancy all of my symptoms decreased, I had an appetite again and was gaining weight. We prepared for a move from Loma Linda back to Los Angeles so that Stephen could focus on his PhD without the long commute, and I extended my leave of absence from medical school. During our apartment hunting we found a lovely 2 bedroom that seemed perfect for starting our family. Unfortunately I experienced my 3rd miscarriage on June 12, 2015. I had a D&C 3 days before we moved, and I was on lifting restrictions. Friends and strangers helped Stephen load and unload the moving van, while I recovered.

I was struggling with depression and my nausea and vomiting had returned. I struggled to get out of bed every day. The 2 bedroom apartment just felt empty, and so did my life. To fill the empty apartment we started renting out our second bedroom to medical students and residents doing rotations in Los Angeles. Sharing my home with strangers seemed scary at first, but I enjoyed having the company of other medical students and being a part of their medical school journey.
I also rescued a feral kitten from the parking lot behind my apartment complex. I already had two cats, which at that time seemed like too many, so I fostered him and my brother and sister-in-law adopted him. They named him Harry after their love for Harry Potter. That started my career as a chronically ill cat lady.
[4 years later, I now have 4 cats, all street rescues, and I foster feral kittens regularly, and I work at a feral cat rescue!]
My health continued to decline into 2016, and my doctors were running out of options.